The Salt Trading Corporation (STC) is all set to celebrate the month of February as the ‘National Iodine month’ .Iodine is a micronutrient essential for thyroid function. Iodized salt prevents goiter, brain damage,and other health problems among children and adults. In line with food and drug regulations, household salt should be fortified with iodine to at least 15 parts per million (ppm) at the consumption level..
The primary strategy for sustainable elimination of iodine deficiency remains Universal Salt Intake. In some countries, however, implementation of salt iodization programmes may not be feasible in all areas, thus resulting in insufficient access to iodized salt for some groups within the population. In these cases, besides strengthening the USI programmes, additional complementary strategies should be considered by the country to ensure optimal iodine nutrition for these susceptible groups. As the first step, countries need to assess and categorize the level of implementation of salt iodization programmes and, based on this analysis, should revisit the strategy for the control of Iodine Deficiency Disorders (IDD), as necessary. Guidance for the categorization and planning process is presented in this statement
Table of Contents
WHO recommendations
1. Countries, or areas within countries, in which more than 90% of the households have access to iodized salt, should sustain the achievement of universal salt iodization (USI) and periodically reassess the salt iodization programme and population iodine status.
2. Countries, or areas within countries, in which 50-90% of the households have access to iodized salt should make efforts to accelerate USI based on the existing operational guidelines (1, 2). If no progress in scaling up is being made within two years, then the feasibility of increasing iodine intake in the form of a supplement or iodine fortified foods by the most susceptible groups – pregnant and lactating women and children 7-24 months of age – would need to be assessed, using the recommended strategy for countries in which 20-50% of the households have access to iodized salt.
3. Countries, or areas within countries, in which 20-50% of the households have access to iodized salt will need to assess the feasibility of increasing iodine intake in the form of a supplement or iodine fortified foods by the most susceptible groups, as described in the following programmatic steps:
- Assess population iodine nutrition status, household iodized salt coverage (preferably disaggregated) and salt iodization programmes in order to identify a national or sub-national problem. An initial rapid assessment will be needed for advocacy and for future monitoring if no assessment has yet been made. The methodology of assessments is described in the WHO/UNICEF/ICCIDD guidelines on “Assessment of Iodine Deficiency Disorders and Monitoring their Elimination” (2).
- Develop new plans to strengthen salt iodization that include increasing political commitment, advocacy, capacity-building of the salt industry for production and quality assurance, adoption and enforcement of appropriate regulations/legislation, and an effective iodized salt monitoring system at production (or importation), retail and community levels.
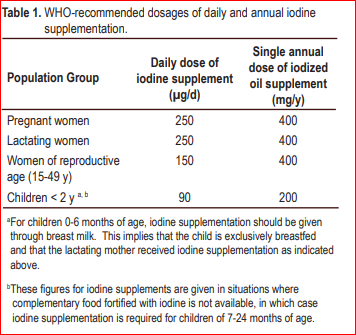
- If a country does not succeed in scaling up its salt iodization programme within two years, the feasibility of increasing the iodine intake of susceptible groups by means of supplements or iodine-fortified foods will need to be explored as a temporary measure while strengthening the salt iodization programme. In areas of moderate and severe iodine deficiency (median urinary iodine less than 50 ug/L or total goitre rate more than 20%), the objective should be to provide additional iodine in the form of a supplement to all pregnant and lactating women, and in the form of a supplement or complementary food fortified with iodine for children 7-24 months of age.
- Assessing the feasibility of providing additional iodine should include: (i) costing of supplementation, (ii) existing channels for distribution to reach the target groups, (iii) likely duration of supplementation, and (iv) potential compliance.
4. Countries, or areas within countries, in which less than 20% of the households have access to iodized salt should assess the current situation of its salt iodization programme to identify national or sub-national problems and to update its strategies and action plans. The most vulnerable groups, pregnant and lactating women, should be supplemented with iodine, and children 7-24 months of age should be given either a supplement or complementary food fortified with iodine until the salt iodization programme is scaled up.

National Status of iodized salt intake
- Ninety-five percent of households use iodized salt for cooking.
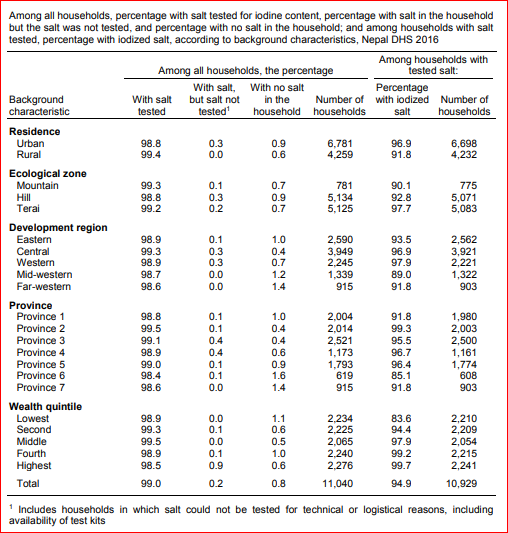
- NDHS 2016 tested for the presence of iodine in household salt by using a rapid test kit. Overall, salt was tested in 99% of the households. Results showed that 95% of the households had iodized salt. The proportion of households with iodized salt is lowest in mountain ecological zone (90%), in Province 6 (85%), and in the lowest wealth quintile (84%).
Iodized Salt (Production, Sale and Distribution)Act, 2055(1998)
It is expedient to make provision for the production, import, supply, sale, distribution of iodized salt in a proper quantity and for mixing iodine with salt in order to prevent and eradicate extensive a nd serious effects caused to public health from iodine deficiency
- Webinar on World Hand Hygiene | Register today
- World’s First 5-in-1 vaccine against meningitis | Men5CV
- World Health Worker Week 2024 | Know theme
- World Autism Awareness Day 2024 | Know theme
- Staff Nurse | OCH | latest jobs vacancy 2024
- World Hepatitis Summit 2024 | WHO
- Staff Nurse | TLMN | ngo jobs 2024
- World Health Day 2024 | Know theme
- Measuring access to assistive technology in Nepal | Country Report
- Migration Health Nurse | IOM | ingo jobs
- Nursing Officer | Kopila Valley | nursing jobs 2024
- Benefits and risks of using artificial intelligence for pharmaceutical development and delivery | WHO
bachelor jobs bph jobs covid19 health health for all health guidelines new health jobs healthjobs healthjobs in nepal health jobs vacancy health public health update ingo jobs jobs after passing bachelor jobs for bph jobs in nepal jobs in ngo ngo jobs ngo jobs vacancy ngo jobs vacancy for bph ngo job vacancy 2021 nurse jobs nurse jobs 2021 nurse vacancy nursing insurance nursing job nursing jobs nursing jobs 2021 nursing jobs in nepal nursing law nursing officer Nursing Vacancy Public health Public health concern public health important days Public health in Nepal publichealth jobs public health updated Staff Nurse Staff Nurse and HA Vacancy | Nepal Army 2021 staff nurse vacancy staff nurse vacancy in ngo 2021 nepal staff nurse vacancy kathmandu who guidelines WHO official

Hey there, I am Nirdesh Baral, founder of Nepal Health Magazine. I am a Tech geek by passion , Public health practitioner by profession and an Ailurophile by heart and a patriot by birth



